What is an allergy?
Hypersensitivity Reaction is a pathophysiological process in which the immune system overreacts to certain foreign substances (called allergens). Normally, the immune system is responsible for recognizing and removing harmful substances such as pathogens, but when the immune system mistakenly regards harmless substances as threats, allergic reactions occur.
Allergens can be divided into four categories according to the route and nature of their invasion into the human body: the first category is inhaled allergens, such as dust mites, pollen, mold and pet dander; the second category is ingestive allergens, mainly food, such as nuts, seafood, milk and eggs; The third category is contact allergens, such as hair dyes, cosmetics and so on.
The fourth category is the injection of allergens, such as drugs;Abnormal immune responses caused by allergens can occur in different organs and parts of the human body, resulting in different symptoms.

What is IgE?
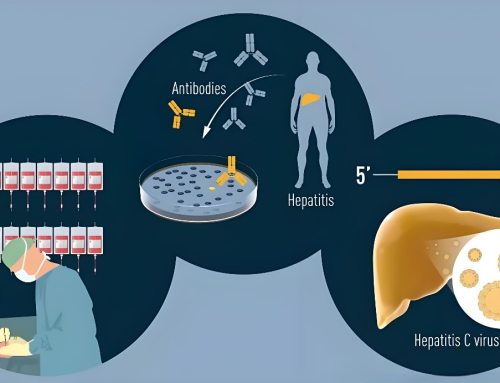
IgE, or Immunoglobulin E, is one of the five major antibody types (IgA, IgM, IgG, IgD, and IgE) in the body’s immune system, and it plays a key role in allergic reactions and immune defenses against parasites. Compared with other types of immunoglobulins, IgE has a very low concentration in the blood, but it plays an irreplaceable role in specific immune responses. IgE is produced by B cells, recognizes and responds to allergens in the environment, and specifically recognizes and binds to specific allergens.
IgE is divided into total IgE and specific IgE (sIgE). Total IgE can roughly reflect whether the patient is allergic, but it is affected by many factors, including heredity, age, infection and immune status, and does not refer to specific allergens. Specific IgE refers to the production of specific allergens, like “a key opens a lock”, which is used to accurately identify allergens.
How is IgE involved in allergic reactions?
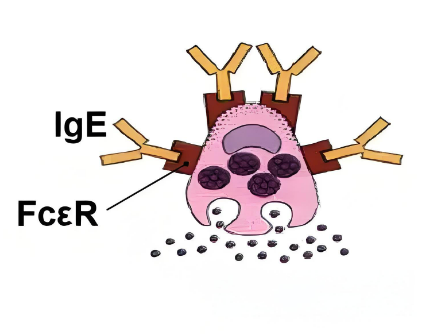
When the human body is first exposed to an allergen (such as pollen, dust mites, pet dander, etc.), the immune system may misidentify it as a harmful substance. In this case, the B lymphocytes begin to produce specific IgE antibodies. These IgE antibodies then bind to receptors on the surface of mast cells (found primarily in connective tissues such as the skin and submucosa of the respiratory tract) and basophils (white blood cells in the blood). IgE antibodies bind to the high affinity receptor (FcεRI) on the cell surface through its Fc segment (the constant region of the antibody), leaving these cells in a “sensitized state”.
When the same allergen is next encountered, the allergen molecule is able to bind to the Fab segment (the variable region of the antibody that is responsible for binding to the antigen) of the IgE antibody immobilized on the cell surface, which is called “cross-linking”. When multiple IgE antibodies are simultaneously “cross-linked” by allergen molecules, the cell membranes of mast cells and basophils are stimulated, triggering cellular degranulation, in which intracellular stores of mediators are rapidly released into the surrounding environment. These mediators include histamine, leukotrienes, prostaglandins, and platelet activating factor, which are potent mediators of inflammation. These released mediators act on the surrounding tissues and organs, causing vasodilation, increased vascular permeability, smooth muscle contraction, etc., leading to allergic symptoms such as skin redness, itching, runny nose, sneezing, asthma attacks, etc
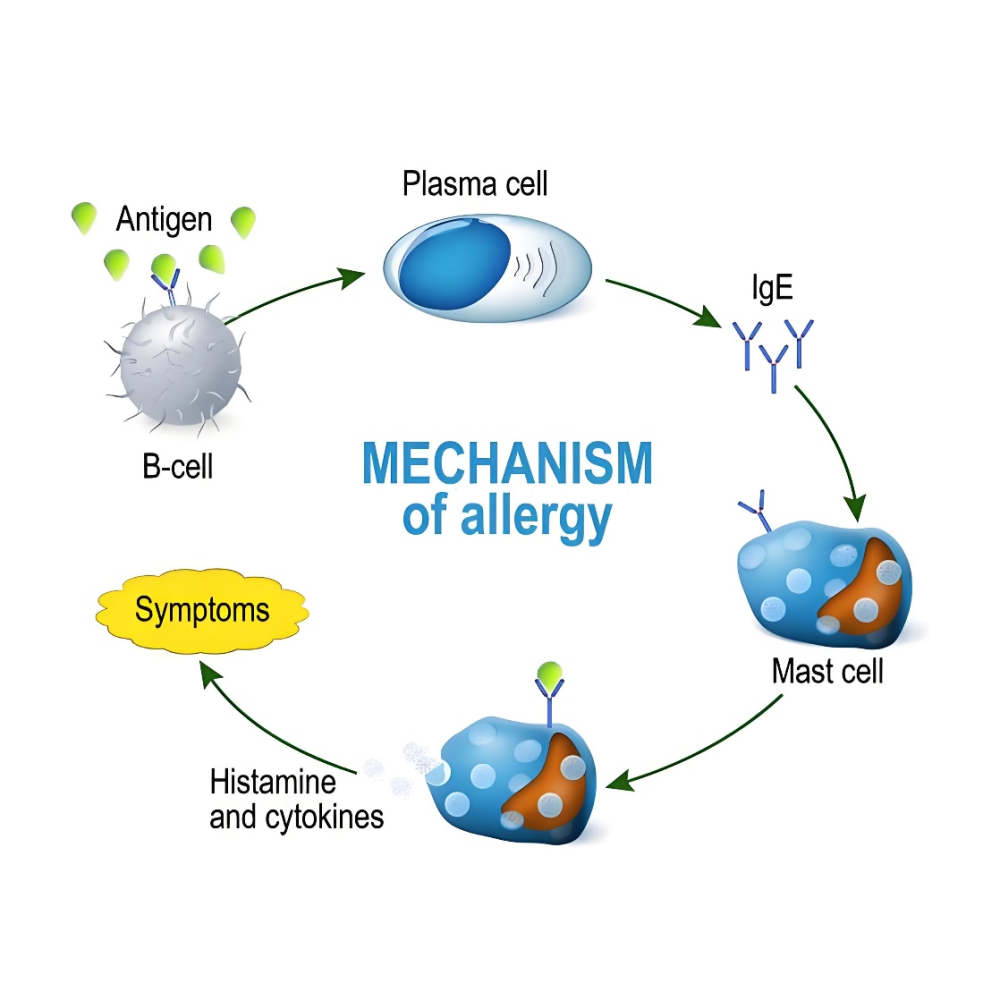
Therefore, IgE plays a “bridge” role in allergic reactions. It not only recognizes and marks allergens, but also acts as a signal transmitter to activate immune cells to release mediators and trigger a series of allergic reactions.
Clinical significance of IgE
Because of its central role in allergic reactions, IgE has important diagnostic and therapeutic implications in the clinic. By measuring IgE levels in the blood, doctors can assess whether a patient is allergic to certain substances and how severe the allergy is. In addition, reducing IgE levels or blocking the interaction between IgE and immune cells is one of the ways to treat some allergic diseases.
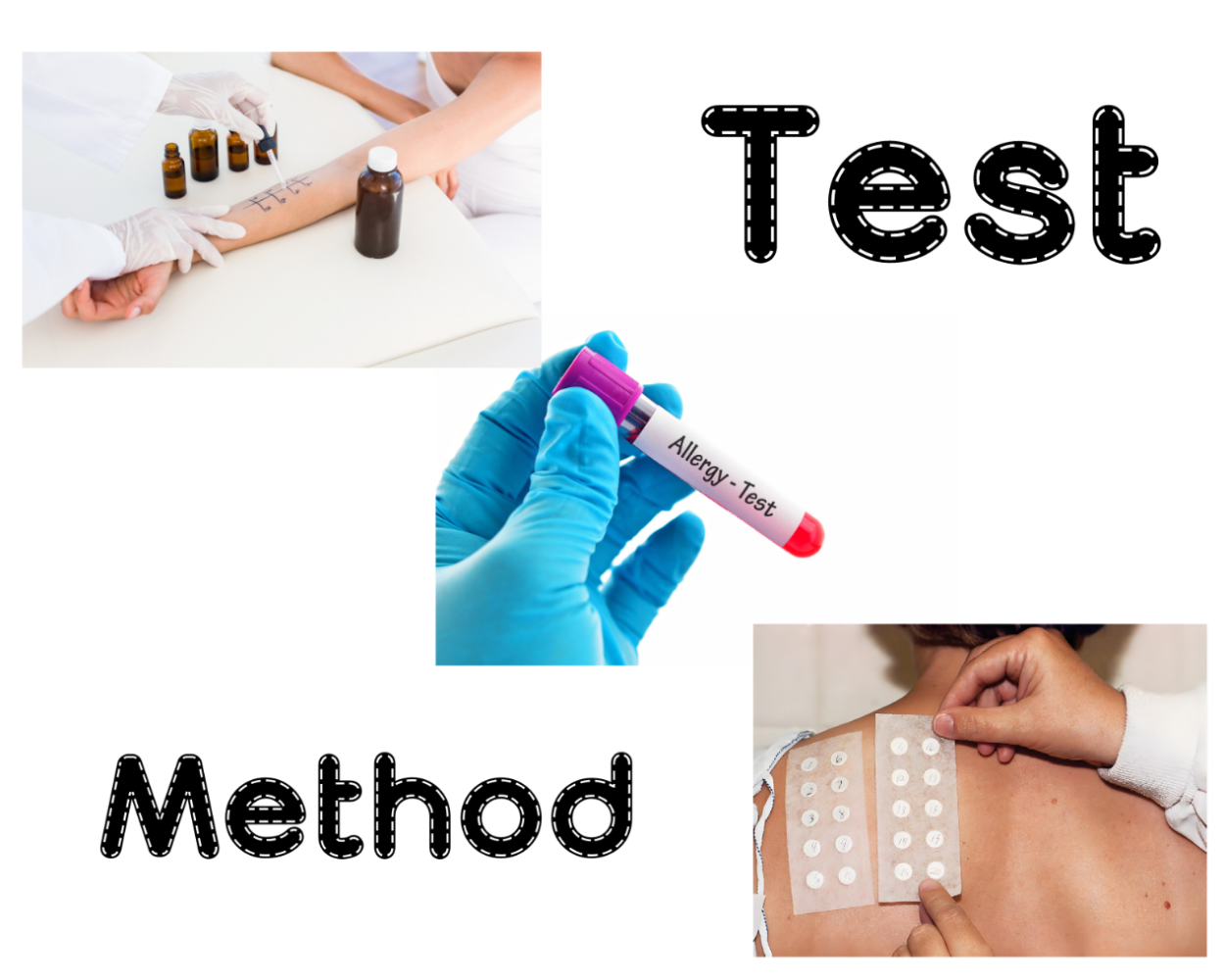
Common detection methods for allergens include:
- Serum-specific IgE testing: By testing blood samples for IgE levels against specific allergens, it is possible to identify precisely which substances an individual is allergic to.
- Prick test: a small amount of potential allergen is applied to the skin to see if it causes a local reaction, so as to determine whether there is an allergy.
- Patch test: mainly used to detect contact allergy, the suspected allergen is placed on the skin for a certain period of time to observe whether there is a rash or erythema. Allergen-specific IgE detection plays an important role in the diagnosis of allergic rhinitis, asthma, eczema, food allergy and other diseases.
Product recommendation
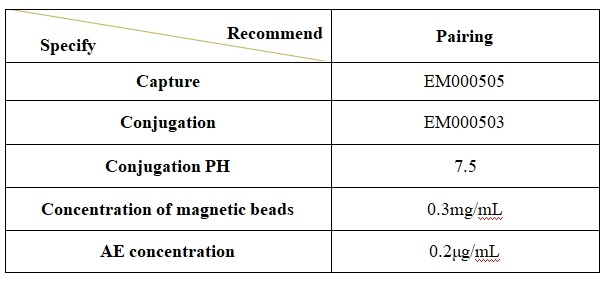
1. Total IgE Recommended Matched Material
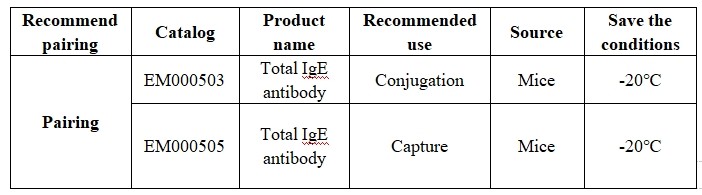
2.Instructions for product use
Product performance demonstration
The comparison results of total IgE and industry benchmark kits are as follows: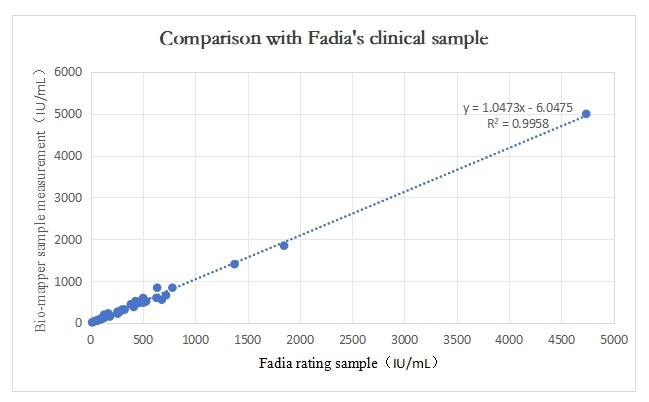
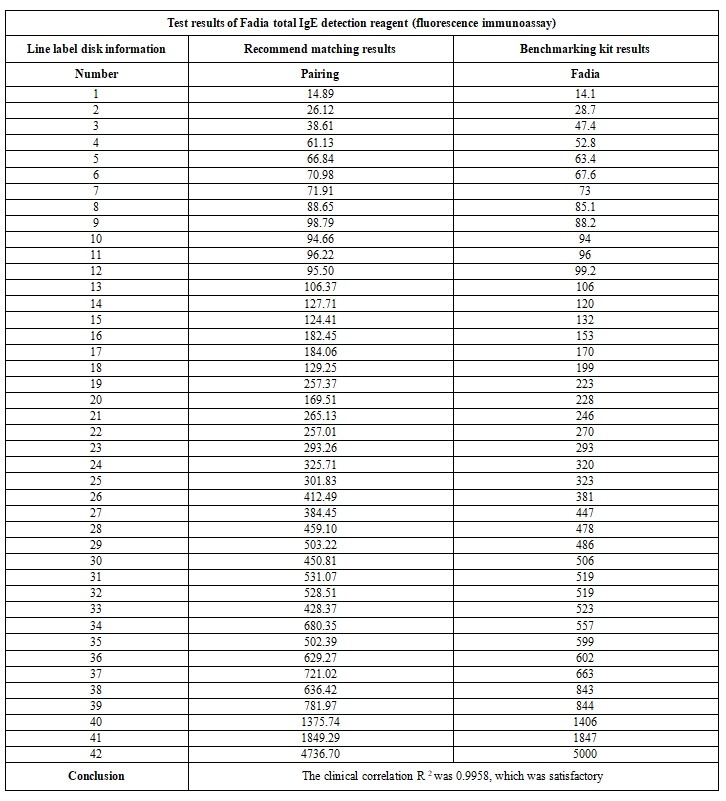
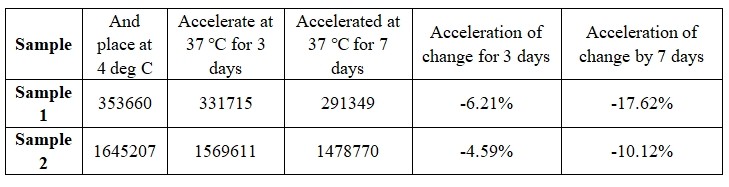
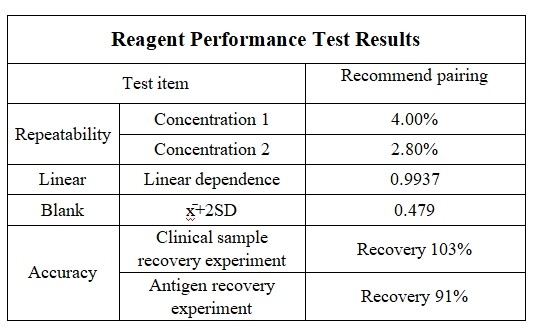
2.Reagent performance result
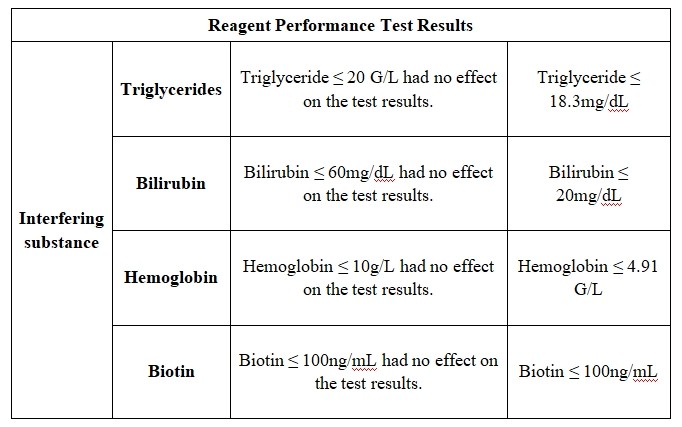
3.Anti-interference performance (sample concentration: 130 IU/mL and 325 IU/mL)
4.Stability of the reagent